Childhood vaccine linked to less severe COVID-19, cigarette smoke raises
risk
 Send a link to a friend
Send a link to a friend
 [November 21, 2020]
By Nancy Lapid [November 21, 2020]
By Nancy Lapid
(Reuters) - The following is a roundup of
some of the latest scientific studies on the novel coronavirus and
efforts to find treatments and vaccines for COVID-19, the illness caused
by the virus.
Childhood vaccine may help prevent severe COVID-19
People whose immune systems responded strongly to a
measles-mumps-rubella (MMR) vaccine may be less likely to become
severely ill if they are infected with the new coronavirus, new data
suggest. The MMR II vaccine, manufactured by Merck and licensed in 1979,
works by triggering the immune system to produce antibodies. Researchers
reported on Friday in mBio that among 50 COVID-19 patients under the age
of 42 who had received the MMR II as children, the higher their titers
-- or levels -- of so-called IgG antibodies produced by the vaccine and
directed against the mumps virus in particular, the less severe their
symptoms. People with the highest mumps antibody titers had asymptomatic
COVID-19. More research is needed to prove the vaccine prevents severe
COVID-19. Still, the new findings "may explain why children have a much
lower COVID-19 case rate than adults, as well as a much lower death
rate," coauthor Jeffrey Gold, president of World Organization, in
Watkinsville, Georgia, said in a statement. "The majority of children
get their first MMR vaccination around 12 to 15 months of age and a
second one from 4 to 6 years of age."

Cigarette smoke increases cell vulnerability to COVID-19
Exposure to cigarette smoke makes airway cells more vulnerable to
infection with the new coronavirus, UCLA researchers found. They
obtained airway-lining cells from five individuals without COVID-19 and
exposed some of the cells to cigarette smoke in test tubes. Then they
exposed all the cells to the coronavirus. Compared to cells not exposed
to the smoke, smoke-exposed cells were two- or even three-times more
likely to become infected with the virus, the researchers reported on
Tuesday in Cell Stem Cell. Analysis of individual airway cells showed
the cigarette smoke reduced the immune response to the virus. "If you
think of the airways like the high walls that protect a castle, smoking
cigarettes is like creating holes in these walls," coauthor Brigitte
Gomperts told Reuters. "Smoking reduces the natural defenses and this
allows the virus to enter and take over the cells."
[to top of second column]
|
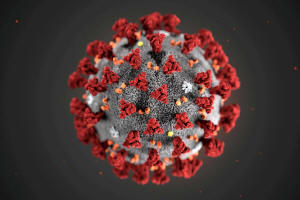
The ultrastructural morphology exhibited by the 2019 Novel
Coronavirus (2019-nCoV), which was identified as the cause of an
outbreak of respiratory illness first detected in Wuhan, China, is
seen in an illustration released by the Centers for Disease Control
and Prevention (CDC) in Atlanta, Georgia, U.S. January 29, 2020.
Alissa Eckert, MS; Dan Higgins, MAM/CDC/Handout via REUTERS.

AstraZeneca's COVID-19 vaccine shows promise in elderly
AstraZeneca and Oxford University's experimental COVID-19 vaccine
produced strong immune responses in older adults in a mid-stage
trial, researchers reported on Thursday in The Lancet. Late-stage
trials are underway to confirm whether the vaccine protects against
COVID-19 in a broad range of people, including those with underlying
health conditions. The current study involved 560 healthy
volunteers, including 240 age 70 or over. Volunteers received one or
two doses of the vaccine, made from a weakened version of a common
cold virus found in chimpanzees, or a placebo. No serious side
effects were reported. Participants older than 80, frail patients,
and those with substantial chronic illnesses were excluded,
according to an editorial published with the study. "Frailty is
increasingly understood to affect older adults' responses to
vaccines," the editorialists write. "A plan for how to consider
frailty in COVID-19 vaccine development is important."
Researchers look into cells infected with new coronavirus
Cells infected with the new coronavirus die within a day or two, and
researchers have found a way to see what the virus is doing to them.
By integrating multiple imaging techniques, they saw the virus
create "virus-copying factories" in cells that look like clusters of
balloons. The virus also disrupts cellular systems responsible for
secreting substances, the researchers reported on Tuesday in Cell
Host & Microbe. Furthermore, it reorganizes the "cytoskeleton,"
which gives cells their shape and "serves like a railway system to
allow the transport of various cargos inside the cell," coauthor Dr.
Ralf Bartenschlager of the University of Heidelberg, Germany told
Reuters. When his team added drugs that affect the cytoskeleton, the
virus had trouble making copies of itself, "which indicates to us
that the virus needs to reorganize the cytoskeleton in order to
replicate with high efficiency," Bartenschlager said. "We now have a
much better idea how SARS-CoV-2 changes the intracellular
architecture of the infected cell and this will help us to
understand why the cells are dying so quickly." The Zika virus
causes similar cell changes, he said, so it might be possible to
develop drugs for COVID-19 that also work against other viruses.
(Reporting by Nancy Lapid, Kate Kelland and Alistair Smout; Editing
by Tiffany Wu)
[© 2020 Thomson Reuters. All rights
reserved.] Copyright 2020 Reuters. All rights reserved. This material may not be published,
broadcast, rewritten or redistributed.
Thompson Reuters is solely responsible for this content. |