Gut bacteria tied to disease severity, immune response; high mental
health toll seen in ICUs
 Send a link to a friend
Send a link to a friend
 [January 14, 2021]
By Nancy Lapid [January 14, 2021]
By Nancy Lapid
(Reuters) - The following is a roundup of
some of the latest scientific studies on the novel coronavirus and
efforts to find treatments and vaccines for COVID-19, the illness caused
by the virus.
Gut bacteria tied to COVID-19 severity, immune response
The microscopic organisms living in our intestines may influence the
severity of COVID-19 and the body's immune response to it, and could
account for lingering symptoms, researchers reported on Monday in the
journal Gut. They found that the gut microorganisms in COVID-19 patients
were very different from those in uninfected individuals. "COVID
patients lack certain good bacteria known to regulate our immune
system," said Dr. Siew Ng of The Chinese University of Hong Kong. The
presence of an abnormal assortment of gut bacteria, or "dysbiosis,"
persists after the virus is gone and could play a role in the
long-lasting symptoms that plague some patients, she said. Her team has
developed an oral formula of live bacteria known as probiotics and a
special capsule to protect the organisms until they reach the gut.
"Compared with patients on standard care, our pilot clinical study
showed that more COVID patients who received our microbiome immunity
formula achieved complete symptom resolution," Ng said, adding that
those who got it had significantly reduced markers for inflammation in
their blood, increased favorable bacteria in their stool and they
developed neutralizing antibodies to the virus.
Pandemic takes toll on ICU workers’ mental health
Nearly half of staff working in intensive care units (ICU) in England
have severe anxiety, depression or post-traumatic stress disorder, with
some feeling they would be better off dead, researchers reported on
Wednesday in Occupational Medicine. The study was conducted in June and
July - before Britain began experiencing its latest surge in
hospitalizations. Among more than 700 healthcare workers in nine ICUs,
45% met the threshold for probable clinical significance for at least
one of four serious mental health disorders: severe depression (6%),
PTSD (40%), severe anxiety (11%) or problem drinking (7%). More than one
in eight reported frequent self-harming or suicidal thoughts in the
previous two weeks. Poor mental health among ICU staff caring for
critically ill and dying COVID-19 patients not only harms their quality
of life but also likely impairs their ability to work effectively, the
researchers said. The findings show an urgent need for mental health
services to be promptly accessible for all healthcare workers.

[to top of second column]
|
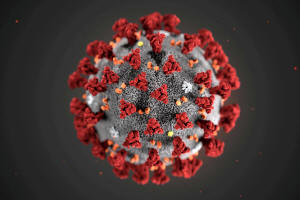
The ultrastructural morphology exhibited by the 2019 Novel
Coronavirus (2019-nCoV), is seen in an illustration released by the
Centers for Disease Control and Prevention (CDC) in Atlanta,
Georgia, U.S. January 29, 2020. Alissa Eckert, MS; Dan Higgins, MAM/CDC/Handout
via REUTERS.

Cooling vests help COVID-19 nurses tolerate PPE
Nurses in COVID-19 wards who wear cooling vests under their personal
protective equipment (PPE) feel less burdened by heat during their
shifts, a small study suggests. Seventeen nurses wore a light-weight
cooling vest under their PPE on one day, and PPE only on another day. On
both days, participants swallowed an electronic capsule that provides a
continuous reading of core body temperature. The vests led to a slight
improvement in body temperature but a much bigger improvement in the
sensation of being too hot, researchers reported in the journal
Temperature. Only 18% of nurses reported thermal discomfort and 35% a
slightly warm thermal sensation at the end of the day with the vest.
That compared to 81% and 94%, respectively, on the day without the vest.
"PPE is known to induce heat stress, which increases fatigue and sensory
displeasure, and is known to impair effective decision making," said
study coauthor Thijs Eijsvogels of Radboud University Medical Center in
the Netherlands. The CoolOver vests made by Dutch company Inuteq are
easy to disinfect and re-activate in a refrigerator, he said, and may
extend work tolerance time and improve recovery of clinicians involved
in COVID-19 care.
Diabetes adds to COVID-19 risks for Black patients
Black patients with Type 1 diabetes (T1D) who become infected with the
new coronavirus face a particularly high risk of a life-threatening
diabetes complication known as ketoacidosis, new data show. T1D usually
develops in children or young adults and requires daily insulin to
survive. Researchers studied 180 patients from across the United States
with T1D and COVID-19, including 31% who were Black and 26% who were
Hispanic. Black patients had nearly four times the odds of developing
diabetic ketoacidosis (DKA) compared with white patients, the
researchers reported in The Journal of Clinical Endocrinology and
Metabolism. Hispanics had a slightly higher risk than white patients.
Blacks and Hispanics were significantly less likely to be using new
diabetes technology like continuous glucose monitoring and insulin
pumps, and had significantly worse blood sugar control compared with
white patients. That suggested that the higher risk was likely driven by
structural and systemic inequality, coauthor Dr. Osagie Ebekozien of the
nonprofit T1D Exchange in Boston told Reuters. Particularly during the
pandemic, healthcare providers need to screen patients with T1D for
socio-economic factors that increase their risk of DKA like food
insecurity, insulin affordability, and access to diabetes supplies, the
researchers said.
(Reporting by Nancy Lapid and Megan Brooks; Editing by Bill Berkrot)
[© 2021 Thomson Reuters. All rights
reserved.] Copyright 2021 Reuters. All rights reserved. This material may not be published,
broadcast, rewritten or redistributed.
Thompson Reuters is solely responsible for this content. |