New kidney problems linked to 'long COVID'; loss of smell may be
followed by other smell distortions
 Send a link to a friend
Send a link to a friend
 [September 04, 2021]
By Nancy Lapid [September 04, 2021]
By Nancy Lapid
(Reuters) - The following is a summary of
some recent studies on COVID-19. They include research that warrants
further study to corroborate the findings and that have yet to be
certified by peer review.
'Long COVID' tied to higher kidney risks
COVID-19 symptoms that persist long after infection, known as "long
COVID", has been tied to a higher risk for new kidney problems,
according to a new study. Analyzing data on more than 1.7 million U.S.
veterans, including nearly 90,000 COVID-19 survivors with symptoms
lasting at least 30 days, researchers found the "long haulers" were at
higher risk for new kidney problems compared to people who had not been
infected with the coronavirus. This was true even when survivors had not
been hospitalized, although declines in kidney function were "more
profound" with more severe infection, they reported on Wednesday in the
Journal of the American Society of Nephrology. Roughly 5% of the Long
COVID group developed at least a 30% drop in a critical measure of
kidney function known as the estimated glomerular filtration rate, or
eGFR. Overall, people with long COVID were 25% more likely than
uninfected people to develop a 30% decline in eGFR, with higher risks in
survivors of more severe disease. While kidney function often declines
with age, the damage in these patients "was in excess" of what happens
with normal aging, study coauthor Dr. Ziyad Al-Aly, of Washington
University in St. Louis, said in a statement. "Our findings emphasize
the critical importance of paying attention to kidney function and
disease in caring for patients who have had COVID-19," he said.

Loss of smell may be followed by smell distortions
Many people who lose their sense of smell due to COVID-19 eventually
regain it, but some survivors later report smell distortions and
unexplained smells, a new study found. Researchers analyzed survey
responses from 1,468 individuals who had been diagnosed with COVID-19
between April and September 2020 and had suffered loss of smell and
taste at the start of their illness. Early on, about 10% also reported
smell distortions, or parosmia, and unexplained smells, known as
phantosmia. At an average of six to seven months after becoming ill and
first reporting loss of smell, roughly 60% of women and 48% of men had
regained less than 80% of their pre-illness smell ability, and rates of
smell distortions and imaginary smells had increased, the researchers
reported on Tuesday on medRxiv ahead of peer review. Roughly 47%
reported parosmia, saying, for example, "some things now smell like
chemicals." About 25% reported phantosmia. "Sometimes I can smell
burning but no one else around me can," one respondent reported.
Persistent smell problems were seen more often in survivors with more
symptoms overall, "suggesting it may be a key marker of long-COVID," the
authors said.
[to top of second column]
|
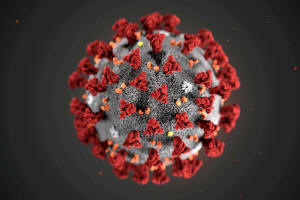
The ultrastructural morphology exhibited by the 2019 Novel
Coronavirus (2019-nCoV), which was identified as the cause of an
outbreak of respiratory illness first detected in Wuhan, China, is
seen in an illustration released by the Centers for Disease Control
and Prevention (CDC) in Atlanta, Georgia, U.S. January 29, 2020.
Alissa Eckert, MS; Dan Higgins, MAM/CDC/Handout via REUTERS

Vaccines induce antibodies despite cancer,
immunocompromise
The mRNA COVID-19 vaccines trigger protective immune responses in
most cancer patients with solid tumors and in many people taking
immunosuppressive medications, two small studies suggest. In Israel,
researchers found that six months after the second dose of the
vaccine from Pfizer Inc and BioNTech SE, 79% of 154 patients with
solid tumors had developed antibodies, as had 84% of 135 similar
people without cancer, a difference that was not deemed
statistically significant. Antibody levels were similar in the two
groups, the researchers reported on Thursday in Cancer Discovery.
Separately, U.S. researchers studied 133 adults taking
immunosuppressive medications for chronic inflammatory diseases and
53 healthy volunteers. At three weeks after the second shot of an
mRNA vaccine from Pfizer/BioNTech or Moderna Inc, nearly 90% of the
immunosuppressed participants had developed antibodies, although
many had lower responses compared to the control group, according to
a report published on Tuesday in Annals of Internal Medicine .
Antibody therapy cuts hospitalization rates
People with mild-to-moderate COVID-19 who were treated with a
monoclonal antibody "cocktail" had lower hospitalization rates than
similar people who did not receive the treatment, researchers
reported on Monday in EClinicalMedicine. They looked at nearly 1,400
such patients, roughly half of whom had received Regeneron
Pharmaceutical Inc's combination monoclonal antibody therapy. Among
those who received the treatment, about 45% were older than 65, and
many had high blood pressure, obesity, diabetes, lung disease and
other risk factors. By four weeks after the treatment, 1.6% of them
had been hospitalized, compared to 4.8% of patients not treated with
the monoclonal antibodies. The study was not randomized and cannot
prove the treatment caused the better outcomes. However, it
"suggests that when patients who are at high risk due to a range of
comorbidities contract a mild or moderate case of COVID-19, this
combination of monoclonal injections gives them a chance of a
nonhospitalized recovery," study leader Dr. Raymund Razonable of the
Mayo Clinic in Rochester, Minnesota in a statement.
(Reporting by Nancy Lapid; Editing by Bill Berkrot)
[© 2021 Thomson Reuters. All rights
reserved.] Copyright 2021 Reuters. All rights reserved. This material may not be published,
broadcast, rewritten or redistributed.
Thompson Reuters is solely responsible for this content.
 |