UN says if US funding for HIV programs is not replaced, millions more
will die by 2029
[July 10, 2025]
By MARIA CHENG
LONDON (AP) — Years of American-led investment into AIDS programs has
reduced the number of people killed by the disease to the lowest levels
seen in more than three decades, and provided life-saving medicines for
some of the world’s most vulnerable.
But in the last six months, the sudden withdrawal of U.S. money has
caused a “systemic shock,” U.N. officials warned, adding that if the
funding isn’t replaced, it could lead to more than 4 million
AIDS-related deaths and 6 million more HIV infections by 2029.
“The current wave of funding losses has already destabilized supply
chains, led to the closure of health facilities, left thousands of
health clinics without staff, set back prevention programs, disrupted
HIV testing efforts and forced many community organizations to reduce or
halt their HIV activities,” UNAIDS said in a report released Thursday.
UNAIDS also said that it feared other major donors might also scale back
their support, reversing decades of progress against AIDS worldwide —
and that the strong multilateral cooperation is in jeopardy because of
wars, geopolitical shifts and climate change.
The $4 billion that the United States pledged for the global HIV
response for 2025 disappeared virtually overnight in January when U.S.
President Donald Trump ordered that all foreign aid be suspended and
later moved to shutter the U.S. AID agency.
Andrew Hill, an HIV expert at the University of Liverpool who is not
connected to the United Nations, said that while Trump is entitled to
spend U.S. money as he sees fit, “any responsible government would have
given advance warning so countries could plan,” instead of stranding
patients in Africa when clinics were closed overnight.

The U.S. President’s Emergency Plan for AIDS Relief, or PEPFAR, was
launched in 2003 by U.S. President George W. Bush, the biggest-ever
commitment by any country focused on a single disease.
UNAIDS called the program a “lifeline” for countries with high HIV
rates, and said that it supported testing for 84.1 million people,
treatment for 20.6 million, among other initiatives. According to data
from Nigeria, PEPFAR also funded 99.9% of the country’s budget for
medicines taken to prevent HIV.
In 2024, there were about 630,000 AIDS-related deaths worldwide, per a
UNAIDS estimate — the figure has remained about the same since 2022
after peaking at about 2 million deaths in 2004.
Even before the U.S. funding cuts, progress against curbing HIV was
uneven. UNAIDS said that half of all new infections are in sub-Saharan
Africa and that more than 50% of all people who need treatment but
aren’t getting it are in Africa and Asia.
[to top of second column]
|
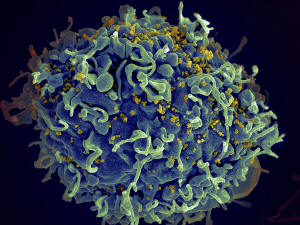
This colorized electron microscope image provided by the U.S.
National Institutes of Health shows a human T cell, in blue, under
attack by HIV, in yellow, the virus that causes AIDS. (Seth Pincus,
Elizabeth Fischer, Austin Athman/National Institute of Allergy and
Infectious Diseases/NIH via AP, File)
 Tom Ellman, of the charity Doctors
Without Borders, said that while some poorer countries were now
moving to fund more of their own HIV programs, it would be
impossible to fill the gap left by the U.S.
“There's nothing we can do that will protect these countries from
the sudden, vicious withdrawal of support from the U.S.,” said
Ellman, director of Doctors Without Borders' South Africa Medical
Unit. “Within months of losing treatment, people will start to get
very sick and we risk seeing a massive rise in infection and death.”
Experts also fear another loss: data. The U.S. paid for most HIV
surveillance in African countries, including hospital, patient and
electronic records, all of which has now abruptly ceased, according
to Dr. Chris Beyrer, director of the Global Health Institute at Duke
University.
“Without reliable data about how HIV is spreading, it will be
incredibly hard to stop it,” he said.
The uncertainty comes as a twice-yearly injectable could end HIV, as
studies published last year showed that the drug from pharmaceutical
maker Gilead was 100% effective in preventing the virus.
Last month, the U.S. Food and Drug Administration approved the drug,
called Sunleca — a move that should have been a “threshold moment”
for stopping the AIDS epidemic, said Peter Maybarduk of the advocacy
group Public Citizen.
But activists like Maybarduk said Gilead’s pricing will put it out
of reach of many countries that need it. Gilead has agreed to sell
generic versions of the drug in 120 poor countries with high HIV
rates but has excluded nearly all of Latin America, where rates are
far lower but increasing.
“We could be ending AIDS," Maybarduk said. "Instead, the U.S. is
abandoning the fight.”
All contents © copyright 2025 Associated Press. All rights reserved
 |