Work requirements could transform Medicaid and food aid under US budget
bill
[May 23, 2025]
By GEOFF MULVIHILL and DAVID A. LIEB
The U.S. social safety net would be jolted if the budget bill backed by
President Donald Trump and passed Thursday by the House of
Representatives becomes law.
It would impose work requirements for low-income adults to receive
Medicaid health insurance and increase them for food assistance as well
as cut funding for services like birth control to the nation’s biggest
abortion provider.
Supporters of the bill say the moves will save money, root out waste and
encourage personal responsibility.
A preliminary estimate from the nonpartisan Congressional Budget Office
said the proposals would reduce the number of people with health care by
8.6 million over a decade.
The measure, which also includes tax cuts, passed the House by one vote
and could have provisions reworked again as it heads to the Senate.
Here's a look at the potential impact.
Work would be required for most people to get Medicaid health
insurance
Starting next year, many able-bodied Medicaid enrollees under 65 would
be required to show that they work, volunteer or go to school in
exchange for the health insurance coverage.
Some people who receive Medicaid were worried Thursday that they could
see their coverage end, even if it is not immediately clear whether they
might be covered by an exception.
Raquel Vasquez, a former cook who is battling two types of cancer and
has diabetes, said she believes she could be affected because she has
not been able to qualify for Social Security disability benefits. “I
cannot even afford this life now because of my disabilities," said the
41-year-old Bakersfield, California, resident. "But my country won’t
even help me.”

About 92% of people enrolled in Medicaid are already working, caregiving,
attending school or disabled. That leaves about 8% of 71 million adult
enrollees who would need to meet the new requirement. An estimated 5
million people are likely to lose coverage altogether, according to
previous estimates of the bill from the Congressional Budget Office.
Only Arkansas has had a work requirement that kicks people off for
noncompliance. More than 18,000 lost coverage after it kicked in 2018,
and the program was later blocked by federal courts.
“The people of Arkansas are generous and we want to help those who
cannot help themselves, but we have no interest in helping those who are
unwilling to help themselves,” said Arkansas Senate President Pro
Tempore Bart Hester, a Republican. “I’m glad the federal government is
starting to align with our thinking.”
Work requirement could hit harder in rural areas
Increased eligibility checks and red tape related to work requirements
may result in some people wrongly getting booted off, said Eduardo
Conrado, the president of Ascension, a health care system that operates
hospitals across 10 states.
That could spell trouble for rural hospitals, in particular, who will
see their small pool of patients go from paying for their emergency care
with Medicaid coverage to not paying anything at all. Hospitals could
have to eat their costs.
“Adding work requirements is not just a policy change, it’s a shift away
from the purpose of the program,” Conrado said of the rule.
That is also a concern for Sandy Heller, of Marion, Massachusetts.
Her 37-year-old son, Craig, has Down syndrome and other complicated
medical needs.
She worries the changes would make it harder for hospitals in
out-of-the-way places like hers to stay afloat and offer the services he
could need.
If they don’t, he would have to travel about 90 minutes for care.
“It could mean life and death for my son if he needed that medical
care,” Heller said.

More people would be required to have jobs to receive food assistance
The Supplemental Nutrition Assistance Program, formerly known as food
stamps, already requires work for some of its roughly 42 million
recipients. Adults ages 18-54 who are physically and mentally able and
don’t have dependents must work, volunteer or participate in training
programs for at least 80 hours a month, or else be limited to just three
months of benefits in a three-year period.
The legislation passed by the House would raise the work requirement to
age 65 and also extend it to parents without children younger than age
7. The bill also would limit the ability to waive work requirements in
areas with high unemployment rates.
[to top of second column]
|
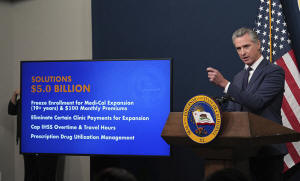
Calif. Gov. Gavin Newsom presents his revised 2025-2026 state
budget during a news conference in Sacramento, Calif., May 14, 2025.
(AP Photo/Rich Pedroncelli, file)
 The combination of those changes
could put 6 million adults at risk of losing SNAP benefits,
according to the liberal-leaning Center on Budget and Policy
Priorities.
Like work requirements for Medicaid, those for SNAP tend to cause a
decrease in participation without increasing employment, according
to an April report by the Brookings Institution’s Hamilton Project.
States that cover immigrants lacking legal status would lose
federal funds
Under the bill, the federal government would punish states that use
their own state dollars to provide Medicaid-covered services to
immigrants lacking legal status or to provide subsidies to help them
buy health insurance.
Some states that provide that sort of coverage extend it only to
children.
Those states would see federal funding for the Medicaid expansion
population — typically low-income adults — drop from 90% to 80%.
That could mean states pull back that Medicaid coverage to avoid the
federal penalty, said Joan Alker, executive director of Georgetown
University’s Center for Children and Families.
KFF said the provision could affect 14 states that cover children
regardless of their immigration status.
This month the Democratic governor of one of them — California's
Gavin Newsom — announced a plan to freeze new enrollments of adults
in state-funded health care for immigrants who do not have legal
status as a budget-balancing measure.
The bill could curtail abortion access by barring money for
Planned Parenthood
Planned Parenthood says a provision barring it from receiving
Medicaid funds could lead to about one-third of its health centers
closing.
The group said about 200 centers are at risk — most of them in
states where abortion is legal. In those states, the number of
Planned Parenthood centers could be cut in half.
Planned Parenthood, the nation’s largest abortion provider, also
offers other health services, including birth control and cancer
screening.
Federal money was already barred from paying for abortion, but state
Medicaid funds in some states now cover it.

“We’re in a fight for survival — not just for Planned Parenthood,
but for the ability of everyone to get high-quality, non-judgmental
health care,” Planned Parenthood President and CEO Alexis McGill
Johnson said in a statement.
Susan B. Anthony Pro-Life America celebrated the provision, saying
“Congress took a big step toward stopping taxpayer funding of the
Big Abortion industry.”
Health services for transgender people would be cut
Medicaid would stop covering gender-affirming care for people of all
ages in 2027 under one provision.
Further, coverage of the treatments could not be required on
insurance plans sold through the exchanges under the Affordable Care
Act.
Trump has targeted transgender people, who make up around 1% of the
U.S. population, since returning to office, including declaring that
the U.S. won’t spend taxpayer money on gender-affirming medical care
for transgender people under 19. The care includes puberty blockers,
hormone therapy and surgeries.
The bill would expand that to all ages, at least when it comes to
Medicaid.
Some states already block the coverage, and some require it. It’s
unclear how much Medicaid has spent on providing gender-affirming
care, which has only been recently added to some coverage plans in
some states.
___
Associated Press reporters Devna Bose in Jackson, Mississippi;
Andrew DeMillo in Little Rock, Arkansas; Susan Haigh in Hartford,
Connecticut; Marc Levy in Harrisburg, Pennsylvania; Amanda Seitz in
Washington; and Leah Willingham in Boston contributed to this
article.
All contents © copyright 2025 Associated Press. All rights reserved
 |